Artigos Originais
Os valores da pressão arterial aórtica e índice de aumentação central em indivíduos com hipertensão da bata branca são mais próximos dos indivíduos normotensos do que dos hipertensos tratados para idênticas idades, género e pressão noturna
Central pressures and central hemodynamic values in white coat hypertensives are closer to those of normotensives than to those of controlled hypertensives for similar age, gender, and 24-h and nocturnal blood pressures
Joana Almeida, José Monteiro, José A. Silva, Susana Bertoquini, Jorge Polónia
Rev Port Cardiol 2016;35:559-67
Conclusions: Our data suggest that for similar age, gender distribution, BMI, and 24-h and nocturnal BP, aortic stiffness, central aortic pressures and wave reflection in WCH are closer to those of NT than to those with treated HT. This supports the idea that white coat hypertension may be a more benign condition than treated hypertension for similar 24-h and particularly nocturnal BP levels.
Disponível online: Português: [Resumo - Texto Completo - PDF]
English: []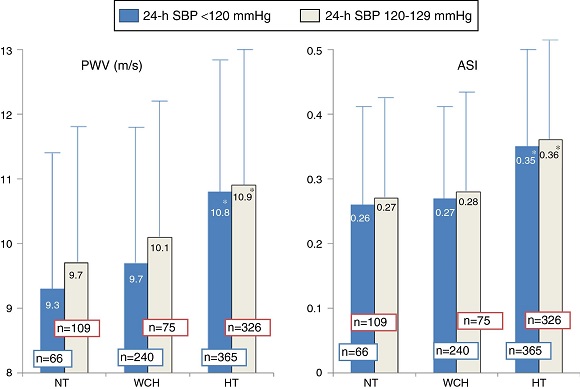
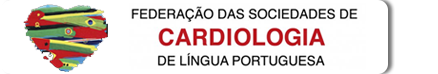
Figure 2. Pulse wave velocity and aortic stiffness index in normotensives (n=175), white coat hypertensives (n=316), and treated hypertensives (n=691), according to 24-h systolic blood pressure <120 mmHg or 120-129 mmHg. The number of individuals in each group is indicated on the corresponding column. ASI: aortic stiffness index; HT: hypertensives; NT: normotensives; PWV: pulse wave velocity; SBP: systolic blood pressure; WCH: white coat hypertensives.
*p<0.04 (significantly different from normotensives and white coat hypertensives in the same group).
Comentário Editorial
A velocidade de onda de pulso, pressão aórtica central e ondas refletidas retrógradas na hipertensão da bata branca
Pulse wave velocity, central aortic pressure, and arterial reflection waves in white coat hypertension
José Mesquita Bastos
Rev Port Cardiol 2016;35:569-71
Conclusions: Almeida et al. found a relatively benign profile of aortic stiffness and central pressures in white coat hypertensives compared to hypertensives, suggesting weaker wave reflections. This cross-sectional study is the first to compare white coat hypertensives, hypertensives and normotensives in which the diagnostic criteria for WCH and hypertension included nocturnal BP values, which have the greatest cardiovascular prognostic value. Further longitudinal studies with greater statistical power are needed to confirm whether WCH is as benign as suggested in this study.
Disponível online: Português: [Resumo - Texto Completo - PDF] English: []
Estenose aórtica calcificada e a sua correlação com um novo marcador inflamatório: a relação linfócito/monócito
Calcific aortic stenosis and its correlation with a novel inflammatory marker, the lymphocyte/monocyte ratio
Tolga Han Efe, Kadriye Gayretli Yayla, Cagri Yayla, Ahmet Goktug Ertem, Tolga Cimen, Hilal Erken Pamukcu, Murat Bilgin, Mehmet Erat, Mehmet Dogan, Ekrem Yeter
Rev Port Cardiol 2016;35:573-8
Conclusions: The present study demonstrated the existence of a statistically significant inverse relationship between severity of calcific aortic stenosis and the lymphocyte/monocyte ratio. The study also revealed that the lymphocyte/monocyte ratio was significantly related to the severity of the aortic valve stenosis process.
Disponível online: Português: [Resumo] English: [Abstract - Full text - PDF]
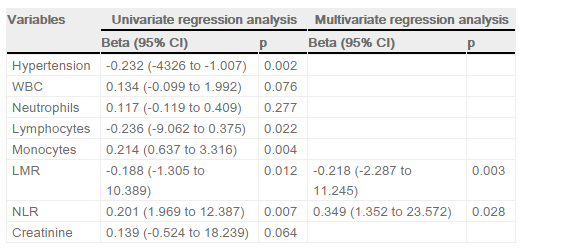
Table 3. Multivariate linear regression analysis showing independent predictors of calcific aortic stenosis severity (mean aortic gradient).
CI: confidence interval; LMR: lymphocyte/monocyte ratio; NLR: neutrophil/lymphocyte ratio; WBC: white blood cell count.
Comentário Editorial
Biomarcadores da estenose valvular aórtica: devemos confiar num único?
Biomarkers of aortic valve stenosis: Should we rely on a single one?
Inês Falcão-Pires, Adelino F. Leite-Moreira
Rev Port Cardiol 2016;35:579-82
Conclusions: As a consequence of rising life expectancy, the demand for aortic valve monitoring can be expected to increase in the future. The initial stages of CAS usually remain asymptomatic for a long time; when patients complain the disease has already progressed to an advanced stage. The more information is gathered on the natural course of aortic valve degeneration, the greater the chances of successfully intervening before irreversible valve damage has ensued and surgery becomes urgent. Therefore, instead of using a single plasma marker, there are high hopes for the potential utility of a panel of biomarkers, reflecting diverse pathways involved in CAS, or even a scoring system that combines biomarkers with echocardiographic and/or clinical data to aid in risk stratification of patients with CAS.
Disponível online: Português: [Resumo] English: [Abstract - Full text - PDF]
Figure 1. Biomarkers of aortic valve stenosis. Ideally a biomarker should be easily measurable, highly reproducible and useful in diagnosing (1), following the disease progression (2) and predicting its prognosis (3). Most of the markers studied so far are valuable tools to diagnose and assess the severity of aortic valve stenosis (AVS, ex. CRP and osteopontin) but show poor utility when it comes to monitor AVS progression or prognosis. The exception seems to be B-type natriuretic peptide (BNP) and its prohormone, NT-proBNP, both able to diagnose, assess the severity and prognosis of AVS patients. BNP mechanism of release is triggered by ventricular pressure overload imposed by the stenotic valve as depicted in the heart on the left. ADMA, asymmetric dimethylarginine; CRP, C-reactive protein; GDF-15, growth differentiation factor-15; hs-CRP, high-sensitivity; tPA, enzyme tissue plasminogen activator. Figure was produced using Servier Medical Art.
Implantação de stent no canal arterial: uma técnica paliativa percutânea promissora em doentes com circulação pulmonar dependente do canal
Ductus arteriosus stenting: A promising percutaneous palliation in patients with duct-dependent pulmonary circulation
Abhishek Raval, Bhavesh Thakkar, Tarun Madan, Nilesh Oswal, Rajiv Garg, Rhshikesh Umalkar, Komal Shah, Bhumika Maheriya
Rev Port Cardiol 2016;35:583-92
Conclusions: Ductal stenting is an effective palliation in patients with duct-dependent PBF. It maintains adequate SO2 and promotes balanced PA growth at mid-term follow-up.
Disponível online: Português: [Resumo] English: [Abstract - Full text - PDF]
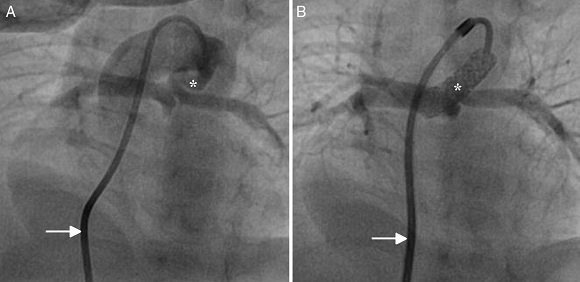
Figure 2. Antegrade ductal stenting in a neonate with pulmonary atresia and ventricular septal defect. (A) Ductal angiogram through a transvenous Judkins right catheter (arrow) showing a tortuous duct (asterisk) arising vertically and proximally from the undersurface of the aortic arch; (B) post-stenting ductal angiogram through a transvenous Mullins sheath and Judkins right catheter (arrow) in the same patient, showing ductal stent with good flow (asterisk).
Alterações eletrocardiográficas em atletas: correlação com a intensidade de desporto e o nível de competição
Abnormal electrocardiographic findings in athletes: Correlation with intensity of sport and level of competition
Hélder Dores, Aneil Malhotra, Nabeel Sheikh, Lynne Millar, Harshil Dhutia, Rajay Narain, Ahmed Merghani, Michael Papadakis, Sanjay Sharma
Rev Port Cardiol 2016;35:593-600
Conclusions: There is a positive correlation between higher intensity of sports and increased prevalence of ECG abnormalities. This relationship persists with the use of more restrictive criteria for ECG interpretation, although the number of abnormal ECGs is lower.
Disponível online: Português: [Resumo] English: [Abstract - Full text - PDF]
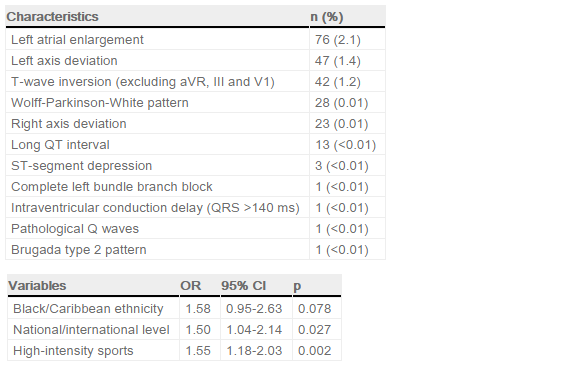
UP: Table 1. Abnormal electrocardiographic changes.
DOWN: Table 3. Independent predictors of abnormal changes according to the Seattle criteria by multivariate analysis (binary logistic regression). (CI: confidence interval; OR: odds ratio.)
Artigo de Revisão
Síndrome cardiorrenal tipo 4
Type 4 cardiorenal syndrome
Ana Luísa Pinheiro da Silva, Manuel Joaquim Vaz da Silva
Rev Port Cardiol 2016;35:601-16
Conclusions: Much remains to be elucidated about type 4 CRS: despite significant progress over the last decade, there are still significant questions regarding its pathophysiology and there is as yet no specific therapy.41 In-depth understanding of the interactions between the heart and kidneys may provide potential targets for intervention.24 These knowledge gaps in the literature constitute opportunities for future research.44 Finally, we emphasize the need to produce guidelines for targeted prevention and effective therapeutic strategies in type 4 CRS: a better understanding of the mechanisms involved in type 4 CRS may provide potential targets for intervention.
Disponível online: Português: [Resumo] English: [Abstract - Full text - PDF]
Casos Clínicos
Valvuloplastia mitral percutânea por balão e encerramento do apêndice auricular esquerdo. Sinergia de dois procedimentos numa única intervenção percutânea
Percutaneous balloon mitral valvuloplasty and closure of the left atrial appendage: Synergy of two procedures in one percutaneous intervention
Daniele Gemma, Raúl Moreno Gómez, Jaime Fernández de Bobadilla, Guillermo Galeote García, Teresa López Fernandez, Jose R. López-Mínguez, José L. López-Sendón
Rev Port Cardiol 2016;35:617.e1-7
Conclusions: Our patient was discharged under chronic oral anticoagulation, since LAA closure does not completely eliminate the risk of embolism in MS patients and she had no contraindications for this treatment. Out of 136 patients who underwent atrial appendage closure during a mitral valve operation, Almahameed et al.8 observed that thromboembolic events were more frequent in patients whose anticoagulant treatment had been stopped after 3.5 years of treatment (10% vs. 15%). The ideal anticoagulant treatment after intracavitary device implantation is unclear, suggesting the use of aspirin in our patient in the three months following the operation.
Disponível online: Português: [Resumo] English: [Abstract - Full text - PDF]
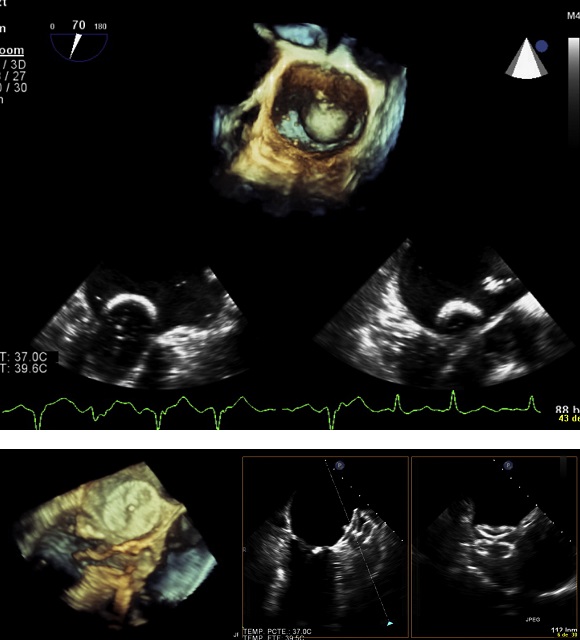
UP: Figure 4. Transesophageal echocardiographic image of percutaneous balloon mitral valvuloplasty.
DOWN: Figure 9. Transesophageal echocardiographic images with three-dimensional reconstruction of the Amplatzer Cardiac Plug in follow-up.
Hipersensibilidade à aspirina e coronariografia urgente: desafio terapêutico
Hypersensitivity to aspirin and urgent percutaneous coronary intervention: A therapeutic challenge
Tatiana Duarte, Sara Gonçalves, Catarina Sá, Rita Marinheiro, Rita Rodrigues, Filipe Seixo, Elza Tomas, Rui Caria
Rev Port Cardiol 2016;35:619.e1-5
Conclusions: Hypersensitivity to NSAIDs is relatively common and constitutes a therapeutic challenge in patients with CAD. Aspirin desensitization appears to b-e effective and safe in most CAD patients, as in the case presented. However, more randomized trials are needed to clarify the risks and benefits. At present, its use should be considered on a case-by-case basis. Desensitization protocols should be established that are appropriate for different situations based on analysis of data from clinical experience, with a view to facilitating decision-making and application.
Disponível online: Português: [Resumo - Texto Completo - PDF] English: []
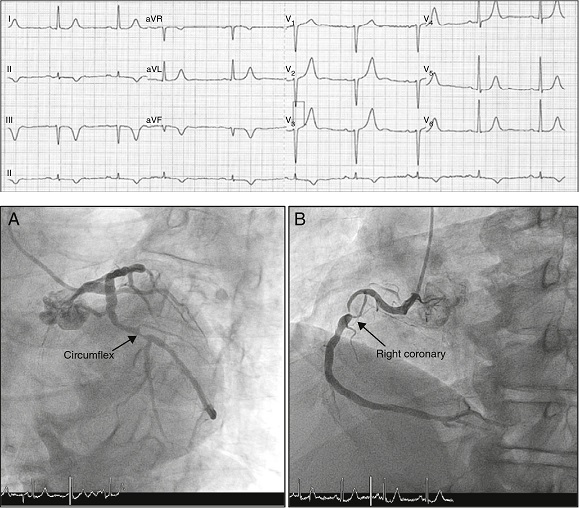
UP: Figure 2. Electrocardiogram showing sinus rhythm, heart rate 60 bpm, new-onset Q waves and deep negative T waves in the inferior leads.
DOWN: Figure 3. Coronary angiography: (A) circumflex with 90% lesion in the proximal segment; (B) right coronary with extensive lesion in the proximal segment, causing severe subocclusive stenosis.
Aneurisma da válvula mitral: uma complicação grave da endocardite valvular aórtica
Mitral valve aneurysm: A serious complication of aortic valve endocarditis
Maria João Sousa, Vasco Alves, Sofia Cabral, Nuno Antunes, Luís Sousa Pereira, Filomena Oliveira, João Silveira, Severo Torres
Rev Port Cardiol 2016;35:621.e1-5
Conclusions: In conclusion, MVAs are rare but potentially life-threatening complications and should be carefully considered in the evaluation of every patient with aortic valve endocarditis. We report a case with impressive images of aortic valve endocarditis complicated by perforated mitral valve aneurysm and severe mitral regurgitation, diagnosed by TEE. This case highlights the importance of early diagnosis with appropriate imaging and timely surgical intervention to prevent fatal outcomes.
Disponível online: Português: [Resumo] English: [Abstract - Full text - PDF]
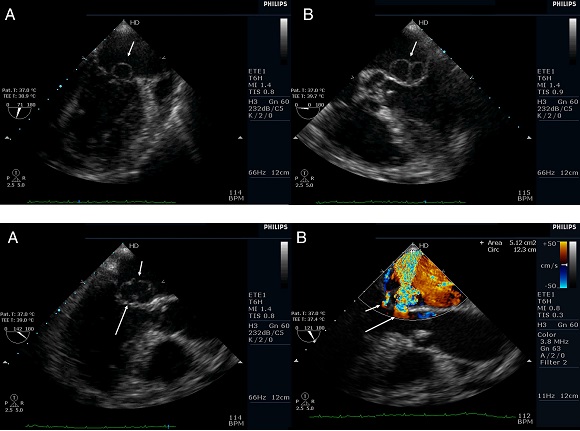
UP: Figure 2. Transesophageal echocardiogram. (A) 2-chamber view: saccular bulge (aneurysm) on the atrial side of the anterior mitral valve leaflet (arrow); (B) 5-chamber view: bilobular image (aneurysm) on the atrial side of the anterior mitral valve leaflet (arrow).
DOWN: Figure 3. Transesophageal echocardiogram (3-chamber view). (A) Ruptured aneurysm of the anterior mitral valve leaflet. The long arrow points to the entry site and the small arrow points to the exit site of the aneurysm; (B) color Doppler image showing two mitral regurgitation jets: a small jet through the leaflet coaptation point (small arrow) and a much more significant one through the aneurysm (long arrow).
Imagens em Cardiologia
Ajuste de plataforma biorreabsorvível em lesão ostial pela técnica de Szabo
Bioresorbable scaffold adjustment in an ostial lesion with the Szabo technique
Carlos Galvão Braga, Raymundo Ocaranza-Sánchez, Santiago Gestal, Ramiro Trillo, José Ramón González-Juanatey
Rev Port Cardiol 2016;35:623-5
Conclusions: To our knowledge, this case reports for the first time the feasibility and safety of the Szabo technique in an ostial lesion with BRS implantation. The use of intracoronary OCT imaging enabled us to ensure and document an excellent result with this technique.
Disponível online: Português: [Resumo] English: [Abstract - Full text - PDF]
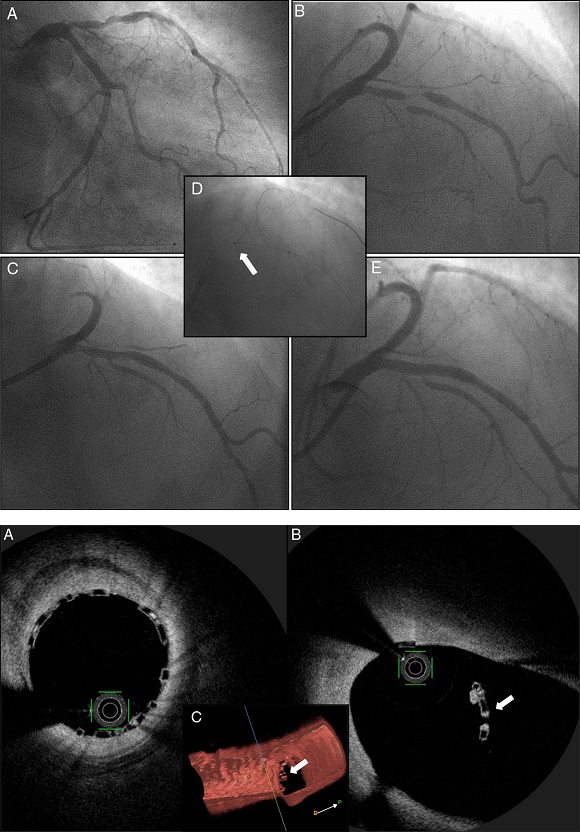
UP: Figure 1. Coronary angiography showing severe disease of the mid left anterior descending (LAD) artery, involving the bifurcation with the first major septal branch (Medina 1,1,1) (A and B); after angioplasty of the first septal branch with a drug-eluting balloon and LAD predilation (C), a bioresorbable scaffold was implanted in the mid LAD using the Szabo technique (D and E).
DOWN: Figure 2. Intracoronary optical coherence tomography revealing optimal strut apposition (A) and the small anchoring strut (white arrow) floating in the circumflex ostium; (B) two-dimensional view from the left anterior descending (LAD); (C) three-dimensional reconstruction, view from LAD.
Pacemaker sem elétrodos: uma mudança no paradigma
Leadless pacemaker: A paradigm change
Nicodemus Lopes, Diogo Cavaco, Pedro Adragão, Pedro Carmo, Francisco Costa, Francisco Morgado
Rev Port Cardiol 2016;35:627-8
Conclusions: Leadless pacemakers represent a paradigm change in pacing. This patient is among the first group of patients implanted with a Micra system in Portugal.
Disponível online: Português: [Resumo] English: [Abstract - Full text - PDF]
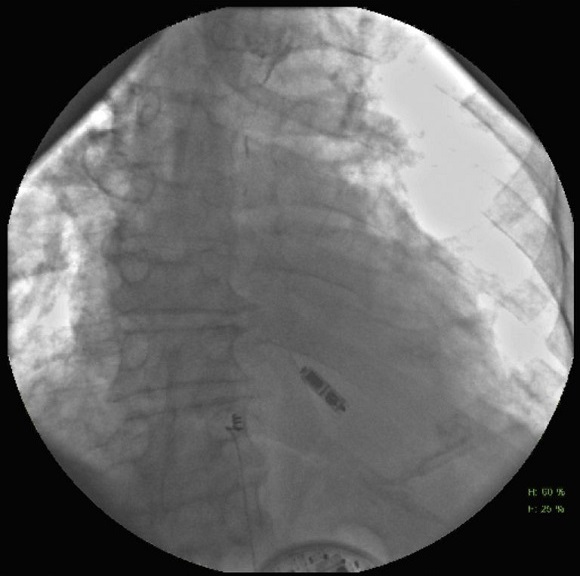
Figure 3. Final position of the leadless pacemaker.
Cartas ao Editor
Ablação de radiofrequência e os preditores para uma recuperação mais rápida para miocardiopatia induzida por taquicardia na população pediátrica
Radiofrequency ablation and predictors for faster recovery for tachycardia-induced cardiomyopathy in the pediatric population
Mustafa Gulgun, Fatih Alparslan Genç, Muzaffer Kursat Fidanci
Rev Port Cardiol 2016;35:629-30
Conclusions: Clinicians should consider tachycardia-induced cardiomyopathy due to PJRT in children and adults with low ejection fraction. Radiofrequency ablation may be a curative treatment for this tachycardia and improvement in left ventricular systolic function is possible after ablation.
Disponível online: Português: [Resumo] English: [Abstract - Full text - PDF]
Resposta à Carta ao Editor «Ablação de radiofrequência e os preditores para uma recuperação mais rápida para miocardiopatia induzida por taquicardia na população pediátrica»
Reply to the letter "Radiofrequency ablation and predictors for faster recovery for tachycardia-induced cardiomyopathy in the pediatric population"
Moisés Rodríguez-Mañero, Javier García-Seara, Jose Luis Martínez-Sande, José Ramón González-Juanatey
Rev Port Cardiol 2016;35:631-2
Conclusions: Hence, in conclusion, from our point of view these case reports are very illustrative because they highlight that catheter ablation of AP in PJRT is an effective and preferable option in patients with tachycardia refractory to multiple pharmacologic treatments, and particularly when left ventricular dysfunction is present. As herein described, it can appear in a wide age range (a newborn1 and an 72-year-old individual2). Finally, although in most cases of PJRT the AP is located in the right posteroseptal region around or just within the coronary sinus ostium,3 other atypical locations such as the one reported in this case are also possible.
Disponível online: Português: [Resumo] English: [Abstract - Full text - PDF]
Artigo Recomendado do Mês
Comentário a «Ultrassonografia para avaliação de água extravascular pulmonar: um novo standard de congestão pulmonar»
Comment on "Ultrasound of extravascular lung water: a new standard for pulmonary congestion"
Dulce Brito
Rev Port Cardiol 2016;35:633-4
Conclusions: As linhas B, usadas por profissionais treinados (sendo o treino fácil) e principalmente «avisados» – em termos de enquadramento clínico e do que se espera ou pretende obter deste sinal ultrassonográfico pulmonar –, são realmente, como referido por Picano E. e Pellikka PA3, um grande ganho diagnóstico a muito baixo «custo» a todos os níveis. Um artigo de revisão a merecer especial atenção.
Disponível online: Português: [Resumo - Texto Completo - PDF] English: [Abstract]
Errata
Errata a «Precisamos do inibidor da P2Y12 como precarga na síndrome coronária aguda sem elevação do segmento ST?»
Erratum to "Do we need P2Y12 inhibitor pretreatment in non-ST elevation acute coronary syndrome?"
Raffaele De Caterinaa, Alessia Delli Veneri
Rev Port Cardiol 2016;35:635
Disponível online: Português: [Resumo] English: [Abstract - Full text - PDF]
Ficha Técnica: Revista Portuguesa de Cardiologia, Volume 35, Número 11, Novembro 2016
A Revista Portuguesa de Cardiologia (RPC) é uma publicação da Sociedade Portuguesa de cardiologia. Fundada em 1982, tem o objectivo de informar e formar os cardiologistas portugueses.
RPC: Diretor - Editor Principal: Lino Gonçalves Subdiretores - Editores Delegados Manuel J. Antunes, Ricardo Seabra Gomes Subdiretores - Editores Associados Manuel Almeida, Nuno Cardim, J. Silva Cardoso, Daniel Ferreira, Victor Gil, Henrique Girão, Mário Oliveira Editor de Suplementos Carlos Aguiar Corpo Redatorial Ana Abreu, Ana G. Almeida, Pedro Antunes, Rui Terenas Baptista, Nuno Bettencourt, Dulce Brito, António Vaz Carneiro, H. Cyrne de Carvalho, Mª da Graça Castro, Diogo Magalhães Cavaco, Cândida Fonseca, Ricardo Fontes-Carvalho, Marco Costa, José Fragata, Ana Galrinho, Cristina Gavina, Alexandra Gonçalves, Pedro Gonçalves, Filipe Macedo, Miguel Mendes, Jorge Mimoso, Eduardo Infante Oliveira, Rui Providência, Evangelista Rocha, Mário Santos, Paulo Sousa, Miguel Sousa Uva Editor de Estatística Adriana Belo Editor de Ética Mário G. Lopes Consultora Editorial e Bibliográfica Helena Donato Tradutor Paul Covill Assessoras Editoriais: Sílvia Gonçalves Silva, Isabel Moreira Ribeiro
Direcção da SPC: Presidente: Miguel Mendes Vice-Presidentes: Nuno Bettencourt de Sousa, Maria João Vidigal Ferreira, Mário Martins Oliveira Secretária-Geral: Regina Ribeiras Tesoureiro: Manuel de Sousa Almeida Secretários-Adjuntos: Pedro Azevedo, Maria Cristina Gamboa, Pedro Pinto Cardoso
Contactos: Campo Grande 28, 13º 1700-093 Lisboa
www.spc.pt | revista@spc.pt | www.spc.pt/RPC | facebook.com/spcardiologia